Understanding and Managing Leg Pain: A Focus on Varicose VeinsLeg pain is a common ailment that affects many people
0 Comments
5 tips to make aortic treatment less invasive:
1. Percutaneous approach for every case! 2. Minimal invasive anesthesia...no intubation! 3. Choose the right stentgraft! 4. Less is more 5. Team work Our team had kept up with the tips and make our most of our elective aortic treatments office procedures. (eBeing a vascular surgeon nowadays, it is imperative to learn to be an endovascualr surgeon. after all, minimal invasiveness is a must for modern doctors performing any kind of treatment.
How to become a competent endovascular surgeon/ interventinist? 1. Believe in endovascular therapy Passion is the fundamental element of being a competent Endovascular surgeon. Passion is everything. You have to from the start believe that endovascular therapy is the right way to do. Most of us have been trained well in open/traditional techniques to solve the clinical problems. However, when you are facing vascular problems nowadays, please do not stick only to the traditional way of treatment. Think over and over again the advantages of endovascular treatment in contrast to traditional cut and shooters, you would then be confident in what you're doing. 2. Be open minded Always be humble. Interventionists are not almighty. We cannot really cure diseases, we help. We are merely doing what we can to improve our patients' quality of life and make them happier. So, stay hungry and foolish. Be ready to listen to the ones who need our help. Endovascular therapy is an art of interaction. Be sure to know the culprit lesion then decide the best/suitable intervention policy. It's not only about giving treatment, it's about communication with the heart of caring. 3. Update! update! update! in this ever hanging world, the rationale, technique and devices evolve so fast that you may miss the catching-up-with easily. With the passion for Endovascular surgery, an Endovasculat surgeon should keep on updating his knowledge on the treatment not only because of his own curiosity but also for the calling deep in his mind. Make sure to read the latest informations, attend up-to-date symposiums and take part in every events (ex. vascular attachment program in CGMH) which may refresh and energize surgeons' concept and technique of patient care. 4. Find your mentor Surgeons learn a lot from clinical practice. And during the practice, we want to minimize the complications as possible. Find a good clinical interventionist as your Endovascular mentor. Try to copy his procedures to treat your patients at your infant stage of clinical practice. Senior staffs' back up are always your patients' safety net. Learn the concept, attitude, technique, and knowledge from your role model in Endovasculat society. And thus the learning curve will be overcome within the shortest period of time. 5. Team work Commending a modern endovascular therapy is like flying a jumbo jet. It takes a good teamwork two make sure that the procedure doesn't go wrong. Multidisciplinary professionals can guarantee to provide the best up-to-date technique in each steps during the whole procedure. Good preoperative study, and comprehensive preprocedure planning, Clea operation image acquisition, dedicate intervention technique, and available surgical bail-outs and back-ups are the keys to the success of modern endovascular procedures. The concept of team work can never be too important for anybody who wants to become a competent endovascular surgeon. Dialysis graft outelt stricture is one of the most frequent complication/situation that a dialysis surgeon faces in his dailiy practice. To cope with the stenotic lesion, the oldest way, probably the most reliable, is to do surgical revision.
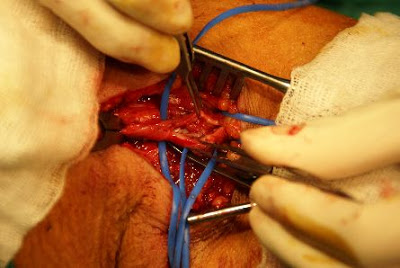
There are two ways of surgical revision of the graft outlet. Here shows the so called" patch angioplasty" method. If the stenotic lesion is a focal or short lesion, we can just longitudinally incise teh graft outlet, and apply a ePTFE patch (which is the same material of the graft) to augment the outelt space. after the operation, the graft outlet should be widely open. The operation usually takes around 1 hour to perform. ofcourse, reoperation sometimes will be troublesome. However, most of the stenotic lesion can be fixed by patch angioplasty. Only if the lesion is too long, then we will try to fix the lesion using a jump graft. Ofcourse nowadays most of the graft outelt stenotic lesion are first treated with angioplasty balloons/ stenting, which is less invasive. However, surgeon should always keep himself familiar with the open procedure. and once the PTA doesnt work, we still can provide a feasible choice of treatment instead of giving up the graft! History
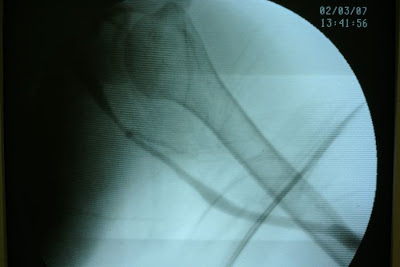
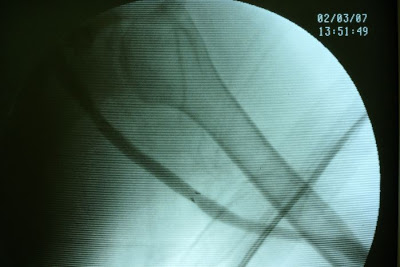
A patietn of ESRD on regular dialysis vie her left upper arm graft. graft outlet segmental stricture was noted and the stenosis was refratory to repeated PTA (percutaneous balloon angioplasty). Operative finding During the venography study, graft outelt segmental stricture was noted. Due to the elasticity of the stricture, definite treatment is needed. Strategy Definite repair of the outlet stricture was needed. The options were: 1. Surgical revision, which is more invasive and time consuming. In addition, the lesion extended up to the high axillary vein make the revision more difficult. General anesthesia was needed to do the jump graft revision which will add on more anesthesia risk. 2. PTA with stent insertion. Covered-stent insertion over the stricture segment can prohibit immediate recoil and may prevent recurrent stricture in the long run. In addition, it's only a percutaneous procedure which is low risk to the patient. Thus we had proceed with covered-stent implantation to deal with the graft outlet recurrent stricture. |
Blog by a
Vascular surgeon in Taiwan AuthorPo-Jen Ko MD Archives
February 2024
Categories |

 RSS Feed
RSS Feed